What is PCOS?
Polycystic Ovarian Syndrome (PCOS) is one of the most common conditions in women of reproductive age, with at least 1 in 10 women diagnosed with PCOS during their lives. This has led to significant interest for women to find information on ways to manage the symptoms. Unfortunately however, there is a lot of misinformation on the topic and has caused a lot of confusion and misdirection for many women.
This article aims to provide honest information, dispel the myths around PCOS and add some practical applications for those with or know someone with this common endocrine disorder.
What causes it?
The direct cause of PCOS is unknown and unfortunately there is no cure. However, it is in part, largely genetic. So, if women in your family have PCOS, there may be an increased chance you can have it. With PCOS being largely genetic, this can account for the wide range of symptoms that appear in women with the condition. In turn, it’s also important to understand that the severity of some symptoms of PCOS are strongly impacted by environmental factors such as your diet, physical activity level and general lifestyle.
How is it diagnosed?
The diagnosis of PCOS, according to Rotterdams criteria are seen when at least 2 out of 3 of the following are true, along with any symptoms previously mentioned:
- Rare or lack of ovulation.
- Biochemical symptoms of hyperandrogenism (increase in male hormones such as testosterone).
- Ultrasound test showing images of polycystic ovaries.
It’s important to note that having one of the following, such as only polycystic ovaries (ovaries that contain a number of harmless follicles (small sacs of fluid)) shown from an ultrasound is not enough to diagnose PCOS.
Symptoms typically include:
- Irregular (cycle falling outside of 21-35 days) or absence of periods.
- Skin issues such as acne
- Difficulty becoming pregnant
- Dark or thick facial and/or body hair (hirsutism)
- Hair loss from the scalp (alopecia)
- Mood disturbances
- Difficulty losing weight
- Depression and anxiety
The longer term risks, which can increase in perimenopausal women, include; infertility, endometrial carcinoma, hypertension, dysfunctional bleeding and possible chronic mental health disorders.
The severity of symptoms can often be seen in those with higher body fat levels. It’s important to note however, that PCOS itself does not lead to an excess in body fat, it is the lifestyle and environmental factors that will determine that outcome. The misconception around this is often down to the presence of insulin resistance in women with PCOS, where many believe that insulin resistance causes weight gain. However, while weight gain causes insulin resistance, insulin resistance does not cause weight gain. An overconsumption of calories (above maintenance/calorie surplus) causes fat/weight gain. Evidence has shown that by reducing body weight by even 5% has shown an improvement in insulin sensitivity and is seen to be a key management strategy for overweight and obese women with PCOS.
Athletes and PCOS
While the prevalence of PCOS is commonly associated with overweight and obese individuals, it is not uncommon for athletes to have PCOS (often referred to as lean PCOS). Menstrual dysfunctions or missed periods are a common occurrence with female athletes and for some this may be down to underfueling and appropriate fueling and professional guidance can generally improve this. Check out our article covering Low Energy Availability here. However for some female athletes, PCOS being a mild form of hyperandrogenism, can lead to irregular menstrual cycles and infertility issues.
Managed PCOS can also offer positive benefits for women in sport with potential performance enhancing benefits in females with PCOS seen in both endurance and power athletes, showing an increase in both muscle and bone mass. Rather than a diagnosis of PCOS being something young females can feel upset about, it could play a positive role in the recruitment of women in competitive sports and a way to avoid the severe symptoms that can come along with unmanaged PCOS.
It’s important to note that women with PCOS are at a higher risk of developing eating disorders potentially due to the pressure to lose weight and being misinformed on ways to achieve this.
Which brings this article to…

5 common PCOS Myths: 👎
1. Everyone with PCOS will be overweight:
A common worry for women is that having PCOS will cause weight gain. As mentioned previously, PCOS does not cause weight gain. It is largely lifestyle modifications and diet that will allow you to maintain a healthy weight.
2. You need to avoid soy based foods
Despite the information and claims to avoid soy based products if you have PCOS, there is currently no scientific data to support claims for either the elimination or restriction of any specific food group or type to improve PCOS symptoms.
3. You must eat Gluten-Free
A common belief from women with PCOS is that they must eliminate gluten from their diet. While this may help some women lose weight, the removal of gluten containing products often leads to a significant reduction in calories, which is what will cause weight loss, not the removal of gluten itself. This weight loss could in turn improve symptoms of PCOS. A very small percentage of women who have gluten sensitivity may feel better from removing gluten from their diet, however not all women with PCOS need to do this. Question your current lifestyle and habits before considering a ‘quick fix’ method to reduce symptoms or weight.
See nutrition recommendations below to help guide you in the right direction.
4. You must avoid Dairy
A common symptom for those with PCOS is skin problems such as acne. Along with this is the common belief that dairy causes these skin issues or enhances the problem. There is however, currently no evidence to support the removal of dairy to improve any PCOS symptoms including acne. For some, a reduction of dairy may improve acne and this will be based on personal trial and error. There is certainly no strong evidence to suggest that every woman with PCOS must eliminate dairy, unless you have an allergy or a high sensitivity. Many other hormonal, nutritional and environmental factors are at play for provoking skin issues.
5. You must avoid carbs
A common belief for women with PCOS is that they must avoid carbohydrates. With insulin resistance being more common in women with PCOS this can make avoiding carbs seem like a good idea. However, this only suggests that eating carbohydrates around exercise or consuming carbohydrate foods along with a protein source may be a better idea. It certainly does not mean eliminating carbs is the best option. Besides, do you really want to give up all those delicious foods when you don’t have to? How long do you think that’s really going to last?

Nutrition 🥗
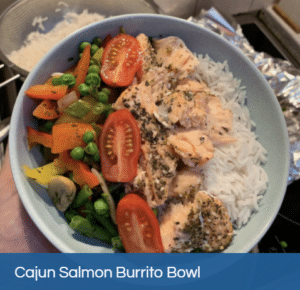
There is no special diet for women with PCOS but rather a well balanced diet and exercise routine, supporting health, can promote a healthy weight and help to reduce the severity of PCOS symptoms. There is some evidence to suggest a mediterranean style diet may help to reduce inflammation and improve insulin resistance. This includes plenty of fruit and vegetables and polyunsaturated fats such as omega 3 fatty acids (almonds, chia seeds, oily fish, flax seeds). Aim for 3-4 servings of fat per day via olive oil, nuts and seeds and oily fish such as salmon 2-3 times per week.
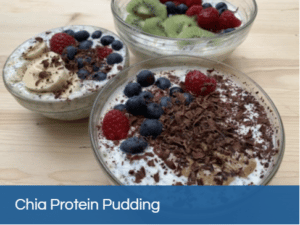
Another key consideration is protein intake. Consuming enough protein can support weight management as it is a filling and satisfying nutrient. It may also play a role in hormone and blood glucose regulation for those with PCOS, so including protein in meals and snacks could help to stabilise blood glucose levels.
Here are some suggestions of snacks & meals to help meet those recommendations:
Supplements: 💊
There are a few supplements that have some evidence to support women with PCOS that are worth considering. Other supplements that you may have read have not been listed, as the evidence is currently not strong enough to support recommendations.
Vitamin D: Deficiency is common in women with PCOS and has been associated with insulin resistance.
Inositol: Studies have shown a beneficial effect of myo-inositol supplement for improving metabolic profile of women with PCOS, potentially reducing hyperandrogenism, supporting ovulation and regulating menstrual cycles.
Reach out to a professional to gain individual supplement dosing recommendations.
Summary: 📝
✅ Choosing lower GI carbohydrates most of the time such as in many of the recipes you’ll find here in the recipe section.
✅ Consuming high protein foods, regularly throughout the day such as meat, seafood, dairy and plant based proteins such as beans, pulses and soya.
✅ Aim to consume a wide variety of fruit and vegetables, and herbs and spices each day.
✅ A good intake of essential fatty acids such as oily fish, almonds, chia seeds and olive oil.
✅ Reach out for support to gain individual advice on weight loss and supplementing.
✅ Lifestyle plays a huge role in the management of PCOS, so staying regularly active, managing sleep, stress and eating a balanced diet all play their part.
Other helpful resources:
What has nature go to do with stress
The Davey Nutrition Guide to Physical Activity for Every Level
References
Balen, A., 2004. The pathophysiology of polycystic ovary syndrome: trying to understand PCOS and its endocrinology. Best practice & research clinical obstetrics & gynaecology, 18(5), pp.685-706.
Hallajzadeh, J., Khoramdad, M., Karamzad, N., Almasi-Hashiani, A., Janati, A., Ayubi, E., Pakzad, R., Sullman, M.J. and Safiri, S., 2018. Metabolic syndrome and its components among women with polycystic ovary syndrome: a systematic review and meta-analysis. Journal of cardiovascular and thoracic research, 10(2), p.56.
Moran, L.J., Ko, H., Misso, M., Marsh, K., Noakes, M., Talbot, M., Frearson, M., Thondan, M., Stepto, N. and Teede, H.J., 2013. Dietary composition in the treatment of polycystic ovary syndrome: a systematic review to inform evidence-based guidelines. Journal of the Academy of Nutrition and Dietetics, 113(4), pp.520-545.
Rotterdam ESHRE/ASRM‐Sponsored PCOS Consensus Workshop Group, 2004. Revised 2003 consensus on diagnostic criteria and long‐term health risks related to polycystic ovary syndrome (PCOS). Human reproduction, 19(1), pp.41-47.