First things first, what is coeliac disease?
Coeliac disease is not an allergy or intolerance. It is an autoimmune condition where the body attacks itself when gluten is eaten and this causes physical damage to the small intestine. This in turn can lead to symptoms and long-term complications if not treated.
Classical symptoms include: bloating, gas, abdominal discomfort, weight loss and diarrhoea. However, there are a number of non-classical symptoms such as dermatitis, brain fog, anaemia, and osteoporosis.
What is Gluten?
Gluten is a protein found in wheat, rye and barley.
Pasta, bread, cakes, biscuits, pastry, some breakfast cereals, certain types of sauces, some ready-made meals, most beers, lagers, and certain fruit squashes. Oats do not contain gluten, however, due to cross-contamination within factories can contain sources of gluten. Therefore, it is advised to use gluten-free oats.
What happens when we eat gluten?
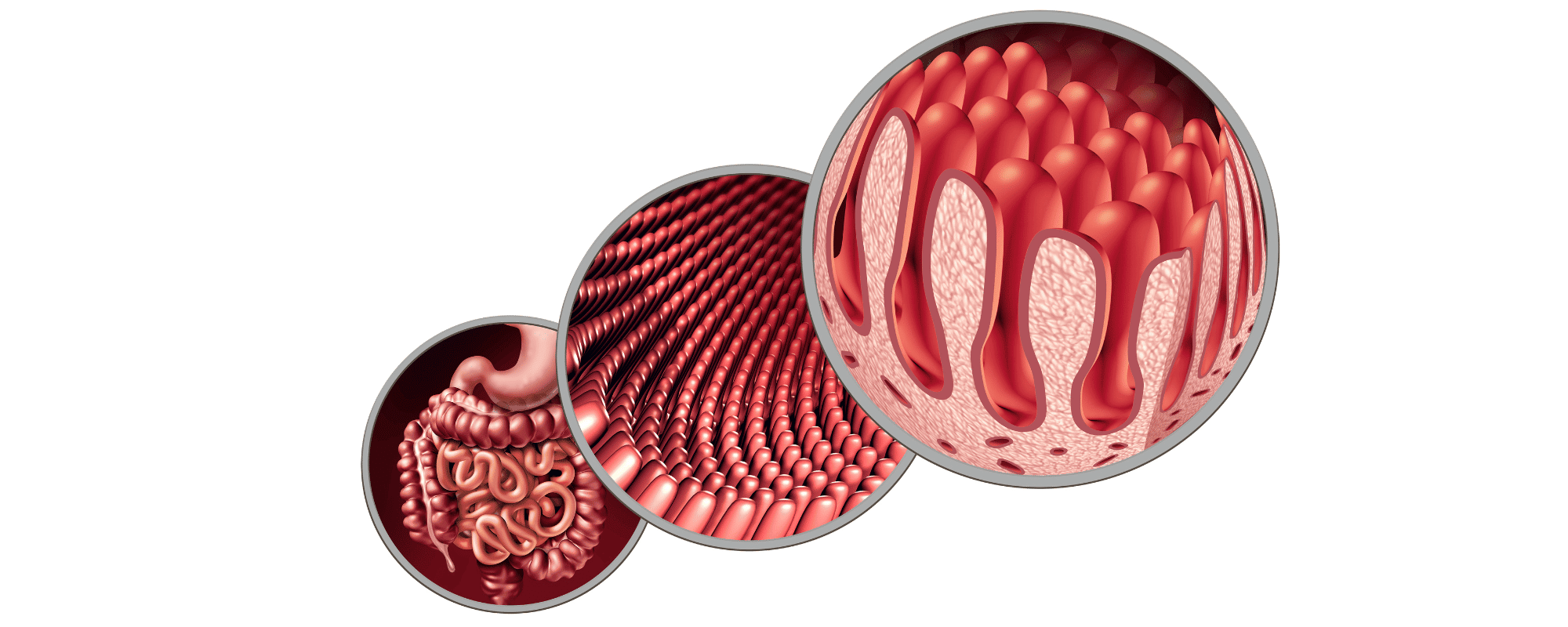
In a healthy gut, you will see finger-like projections (villi), they absorb vitamins/ minerals into the bloodstream. When you have coeliac disease and you eat gluten it causes physical damage to the villi of the small intestine- flattening the villi, which impacts the gut’s ability to absorb vitamins/ minerals. This can lead to malnutrition, definitions, anaemia, low iron, fatigue etc.
Some people can be sensitive to gluten without being coeliac and suffer with symptoms such as bloating, gas, abdominal discomfort, weight loss and diarrhoea, similar to those experienced by a person with coeliac disease, but generally less severe. Symptoms improve when gluten is eliminated from the diet. This is often referred to as ‘gluten intolerance’ and common among those with Irritable Bowel Syndrome (IBS) in particular. Studies have shown however that the reason those with IBS often feel better and experience less bloating and abdominal discomfort is because grains that contain gluten are also high in fructans (gas producing fermentable sugars). Therefore there may not be a need to eliminate gluten from the diet, but rather limit the intake of fructans or other FODMAP foods if you notice that they trigger these symptoms (Skodje et al., 2018). The vegetables that contain high amounts of fructans include artichoke, leek, onion, garlic. Other foods such as wheat pasta, wholemeal bread, rye bread, muesli containing wheat, rye crispbread, cashew nuts, macadamias, peanuts and pine nuts also contain fructans which may trigger symptoms (Monash University).
If you are experiencing symptoms of coeliac disease, gluten sensitivity or ongoing gut related issues, it is recommended that you visit your GP and consider working with a Dietician. The elimination of certain foods from your diet to alleviate symptoms should be done with the support and guidance of a qualified Dietician to ensure that you are meeting your energy and nutritional needs.

When to see a GP
You have been bloated for 3 weeks or more
Regularly bloated (12 or more times per month)
Lifestyle and dietary changes have not improved your symptoms
Other symptoms such as nausea, diarrhoea, constipation, weight loss or blood in your stool
Your symptoms are impacting your quality of life
Coeliac Disease Diagnosis
You should follow up on your symptoms and be tested for coeliac disease if you have any one of the following:
- Severe or persistent mouth ulcers
- Prolonged and frequent fatigue
- Stunted growth
- Unexplained and recurring GI symptoms – nausea, vomiting, stomach pain
- Nutrient deficiencies that are unexplained – particularly in iron, Vitamin B12 or folate
- Type 1 Diabetes
- Autoimmune thyroid disease – under or overactive thyroid (hypothyroidism or hyperthyroidism)
- Irritable Bowel Disease (IBS)
- Numbness or tingling in hands or feet (peripheral neuropathy)
- Difficulty with co-ordination, balance or speech
- Immediate family member with coeliac disease
Testing for coeliac disease involves blood tests and a biopsy of the small intestine. The biopsy will involve an endoscopy of the small intestine, also referred to as oesophagogastroduodenoscopy (OGD).
Blood tests can be carried out by your GP to test for antibodies (IgA, IgA tTGA and IgA EMA). If raised tTG or positive EMA levels are identified then your GP will refer you for a biopsy with a gastroenterologist. It is important that you do not eliminate gluten from the diet before these blood tests as doing so could give incorrect results. The aim of the blood test is to investigate the bodies response to gluten by testing the presence of the relevant antibodies
What if my blood tests are normal?
Normal blood results can occur in those with the disease and so an OGD may be required for accurate diagnosis of coeliac disease. This happens in a small number of people who have coeliac disease but are deficient in IgA.
Unfortunately, up to 75% of people with the disease go undiagnosed and it takes an average of 13 years to get diagnosed. Therefore, if you do receive normal blood results but your symptoms are persistent and negatively effecting your quality of life, it is important that you follow up the investigation with a biopsy.
How does the biopsy diagnose the disease?
A biopsy is a more conclusive means of diagnosing the disease. During the OGD/biopsy, a small tube with a light and camera on the end is passed down through the mouth into the small intestine (duodenum or jejunum), to collect a small piece of tissue from the intestinal wall. The tissue is then taken for examination to identify if the person has coeliac disease. A person with the disease will present with damaged intestinal villi.
What does the biopsy involve?
You will attend an outpatient department after fasting overnight. It will take about 15 minutes for the procedure and you will often be lightly sedated for it to help you relax and given a local anaesthetic to numb the throat. There is no pain experienced however, kids will usually receive a general anaesthetic for the procedure.

I am waiting for my results after being tested for coeliac disease, what should I do?
While you are waiting for your results, it is not recommended to eliminate gluten from your diet until the diagnosis is confirmed. Continue with your regular diet and take care to reduce or avoid foods that you know give you discomfort. See our article on bloating management for tips on how to manage some symptoms of gut discomfort.
Bloating – What is it and why is it happening? – daveynutrition
Bloating: Management guide – daveynutrition
I have been diagnosed with coeliac disease, what now?
If and when you are diagnosed with the disease, it is advised that you work with a registered dietician to eliminate gluten containing foods from your diet. In a recent study, it was found that only 51% of individuals who are diagnosed with coeliac disease are referred to a dietician (Venkateswaran et al., 2022). Working with a Dietician to make the necessary changes to your diet will help you to avoid or amend nutrient deficiencies and ensure you are meeting your nutritional needs.
You may need further testing for other associated conditions such as vitamin deficiencies (ie. iron deficient anaemia, vitamin B12 deficiency or folate deficient anaemia). If the condition is suspected to have affected your bones due to poor nutrient absorption, you may be advised to get a DEXA scan to assess if you are at risk of bone fractures, osteopenia or osteoporosis.
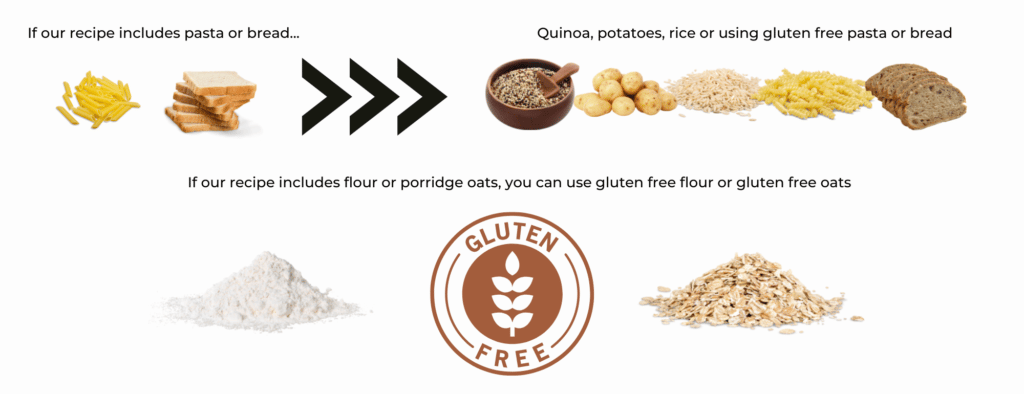
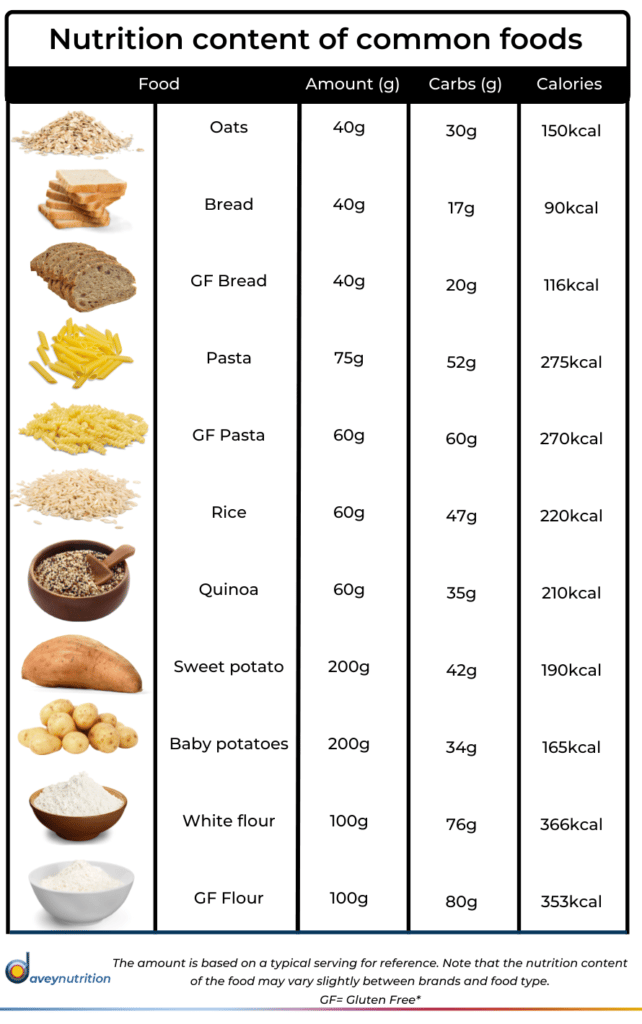
Can I still use the daveynutrition recipes on a gluten-free diet?
The majority of our recipes are actually gluten free however those that are not, can easily be adapted to suit your nutritional needs. Here is our guide to how you can use our recipes and meal plans, on a gluten free diet:
Useful websites:
FODMAP food list | Monash FODMAP – Monash Fodmap
Coeliac disease – Diagnosis – NHS
Getting Diagnosed – Coeliac Society Of Ireland
Coeliac Disease – Eat Well by Sarah Keogh, Dietitian & Nutritionist
References
Caio, G., Volta, U., Sapone, A. et al. coeliac disease: a comprehensive current review. BMC Med 17, 142 (2019). https://doi.org/10.1186/s12916-019-1380-z
Leonard MM, Sapone A, Catassi C, Fasano A. coeliac Disease and Noncoeliac Gluten Sensitivity: A Review. JAMA. 2017;318(7):647–656. doi:10.1001/jama.2017.9730
Skodje, G. I., Sarna, V. K., Minelle, I. H., Rolfsen, K. L., Muir, J. G., Gibson, P. R., Veierød, M. B., Henriksen, C., & Lundin, K. (2018). Fructan, Rather Than Gluten, Induces Symptoms in Patients With Self-Reported Non-Celiac Gluten Sensitivity. Gastroenterology, 154(3), 529–539.e2. https://doi.org/10.1053/j.gastro.2017.10.040