Introduction and key points:
Gastrointestinal (GI) symptoms are highly variable between individuals and depend on a number of factors including exercise duration, intensity and nutrition and hydration strategies.
- Symptoms tend to occur more frequently with longer duration / higher-intensity activities and can be caused by (but are not limited to) 3 main reasons: mechanical, physiological or nutritional reasons.
- The main cause of symptoms seems to be reduced blood flow to the gut which can be caused by a number of reasons.
- Part 2 of this series of articles will examine management strategies to reduce the incidence and severity of symptoms.

Funny tummy? Bloating? Cramps? Needing ‘to go’? As an athlete you may have experienced one or all of these symptoms among others before, during or after training or an event. Gastrointestinal issues are a frequent occurrence among athletes, particularly endurance athletes but can occur in athletes involved in any sport or people who do not consider themselves an athlete but are physically active. Symptoms can often cause discomfort, pain and even lead to unfinished events and competitions and it is important to understand why certain symptoms occur for you and how to minimise the impact and severity of these symptoms as much as possible.
What is the gut and how does it impact on our performance as an athlete?
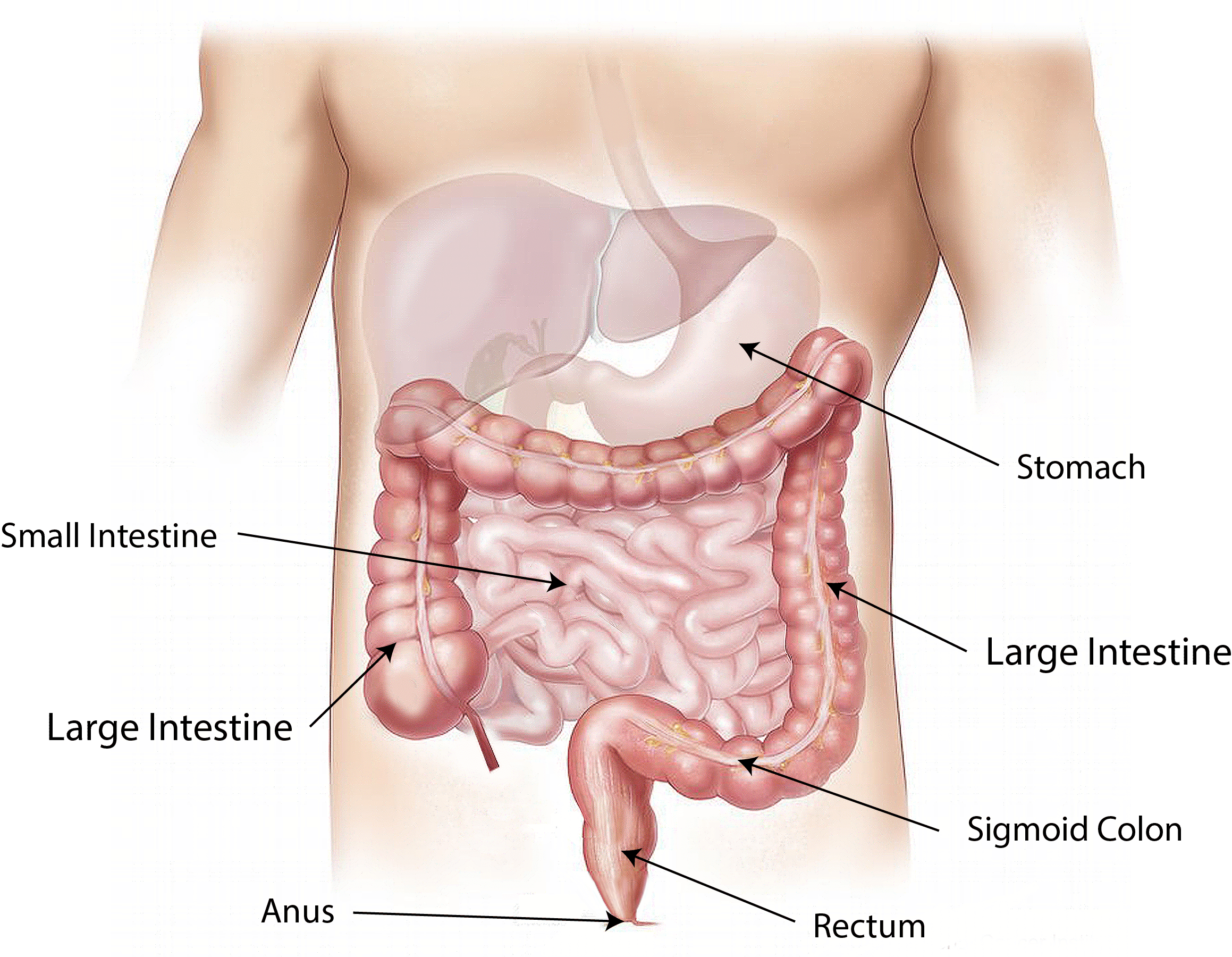
The gastrointestinal tract (‘GI tract’ or ‘gut’) is a tube or passageway in the body which begins at the mouth and ends at the anus. It includes the oesophagus, stomach, small and large intestine and rectum. The function of the GI tract is to allow foods to be transported, digested and absorbed.
 Some of the reported symptoms associated with exercise and GI distress include belching, heartburn, reflux, cramps in the stomach, bloating, feeling nauseas, vomiting, diarrhea, flatulence and feeling an ‘urge’ to go to the toilet.
Some of the reported symptoms associated with exercise and GI distress include belching, heartburn, reflux, cramps in the stomach, bloating, feeling nauseas, vomiting, diarrhea, flatulence and feeling an ‘urge’ to go to the toilet.
Symptoms experienced by athletes can vary between individuals and in relation to the duration and intensity of the exercise. In addition, athletes have reported experiencing one or more of the symptoms with no clear patterns associated with different activities. The main underlying cause of most exercise-induced GI symptoms seem to be associated with a reduced blood flow to the gut and can be best managed over time with optimal training, nutrition and hydration strategies.

There are three main reasons why symptoms may occur but it is important to note that this list is not exhaustive and other reasons may cause individuals to experience varying degrees of one or more symptoms.
1) Physiological reasons:
These can occur due a reduction in blood flow to the gut as blood is directed towards the working muscles involved in that exercise. For example, during a run more blood will be sent to the legs as this is where it is needed most. From an evolutionary point of view the body sees the movement as either a) movement to get food or b) running from danger! So it is no wonder that we preferentially will send the blood to the working muscles – survival mode!
When there is a lack of blood flow (carrying essential oxygen and nutrients) the gut cannot function as it should which can lead to symptoms and damage.
Some athletes may also experience feelings of stress and/or anxiety in the lead up to a competition which can lead to gut issues. The gut has been referred to as ‘the second brain’ because of the vast number of neurons it contains which pass information to the central nervous system. In addition, information will be passed from the central nervous system to the gut and this can be referred to as the ‘gut-brain connection (or axis)’.if you have anxious thoughts in the lead up to an event, you can often ‘feel’ these in your gut and the anxiety can manifest as gut symptoms. Psychological stress can cause the blood to be redirected from the gut and slow stomach emptying which may cause an increase in the severity/duration of certain symptoms.

2) Nutritional reasons:
Certain nutrients can cause gut issues if consumed too close to training and/or an event. These include protein, fibre, fat and fructose (a type of carbohydrate) and dairy products however this varies hugely between different athletes. These may cause issues when consumed too close to, during or directly after an event or training.
It has been reported that some drinks containing more than 12g of carbohydrate per 100ml plus electrolytes may cause issues for individuals. During intense exercise the rate of digestion is much lower at just 6g per 100 ml solution (the amount of carbohydrate in a commercially produced sports drink). Athletes are recommended to consume 60 g of carbohydrate per hour during intense exercise, in an easily digestible form, to avoid gastro intestinal issues.
Dehydration has also been shown to cause some issues as lack of water can impact on blood volume and the delivery of blood to the gut, reducing blood flow further.

3) Mechanical reasons:
These seem to occur more frequently during exercise which is higher impact (eg: long distance running) whereby there is a repetitive ‘bouncing’ movement which can cause damage to the intestinal walls.In conjunction with this damage, there is reduced blood flow to the gut which may cause bleeding and long distance runners have reported blood in stool at the end of an event. Longer distance and/or higher intensity exercise are associated with an increase in symptoms. Some cyclists may also experience GI symptoms as a result of their positioning and posture on a bike which can put pressure on the abdomen and lead to uncomfortable symptoms.

Symptoms are highly individual but can be managed. Stay tuned for Pt. 2 of this series to understand how to apply practical management strategies and minimise the duration and/or severity of potential gut issues.
References:
de Oliveira, E.P., Burini, R.C. and Jeukendrup, A., 2014. Gastrointestinal complaints during exercise: prevalence, etiology, and nutritional recommendations. Sports Medicine, 44(1), pp.79-85.
Jeukendrup, A.E., 2011. Nutrition for endurance sports: marathon, triathlon, and road cycling. Journal of sports sciences, 29(sup1), pp.S91-S99.
Jeukendrup, A., 2013. The new carbohydrate intake recommendations. In Nutritional Coaching Strategy to Modulate Training Efficiency (Vol. 75, pp. 63-71). Karger Publishers.
Jeukendrup, A.E., 2017. Training the gut for athletes. Sports Medicine, 47(1), pp.101-110.
Kerksick, C.M., Arent, S., Schoenfeld, B.J., Stout, J.R., Campbell, B., Wilborn, C.D., Taylor, L., Kalman, D., Smith-Ryan, A.E., Kreider, R.B. and Willoughby, D., 2017. International society of sports nutrition position stand: nutrient timing. Journal of the International Society of Sports Nutrition, 14(1), pp.1-21.
Lambert, G.P., Lang, J., Bull, A., Eckerson, J., Lanspa, S. and O’Brien, J., 2008. Fluid tolerance while running: effect of repeated trials. International journal of sports medicine, 29(11), pp.878-882.
Lis, D.M., Stellingwerff, T., Kitic, C.M., Fell, J.W. and Ahuja, K.D., 2018. Low FODMAP: a preliminary strategy to reduce gastrointestinal distress in athletes. Medicine & Science in Sports & Exercise, 50(1), pp.116-123.
Staudacher, H.M., Irving, P.M., Lomer, M.C. and Whelan, K., 2014. Mechanisms and efficacy of dietary FODMAP restriction in IBS. Nature reviews Gastroenterology & hepatology, 11(4), p.256.









